Duke OBGYN
fighting confusion around employment laws for pregnant people in the workplace.
Duke OBGYN needed an employment law training video that could make complex legal guidance clear and informative for healthcare providers. We partnered to design and produce a training video that turns dense legal guidance into practical, usable content for healthcare teams.
By creating a resource clinicians can trust, the work supports more confident conversations around pregnancy and workplace policies.
This project builds on our experience designing provider education across healthcare, including healthcare training video for Safe Sleep NC and education toolkit for I Gave Birth Initiative. It reflects how we design training and communication tools for healthcare teams navigating complex, high-stakes topics.
Video transcript
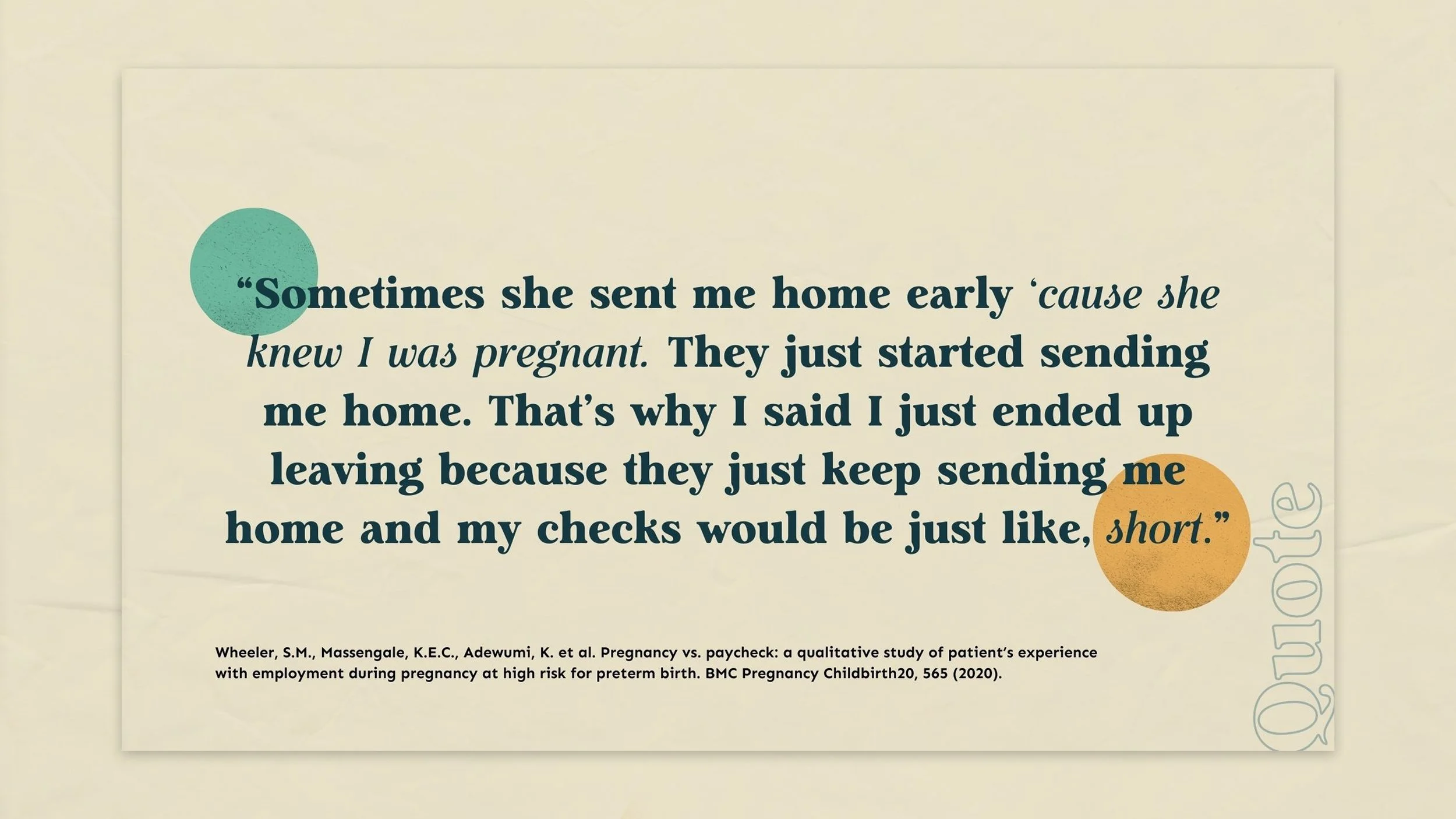
Welcome to the Preparing Obstetric teams to promote equity in employment or promote clinical team member training. Sometimes she sent me home early 'cause she knew I was pregnant. They just started sending me home. That's why I said I just ended up leaving because they just keep sending me home and my checks would be just like short.
Both in our work and the lay press, there are numerous examples of likely well-meaning clinicians providing documentation that backfired resulting in lost wages or even termination. We developed this training with the goal to empower obstetric clinical team members with the basic knowledge needed to counsel patients and provide documentation when it is needed.
We know that obstetric team members have so many things to cover during each prenatal visit. And you're not a lawyer or a human resources specialist. We've designed this training to be practical and to give you basic information so that you can accurately counsel patients and you can direct them to additional resources when it's needed.
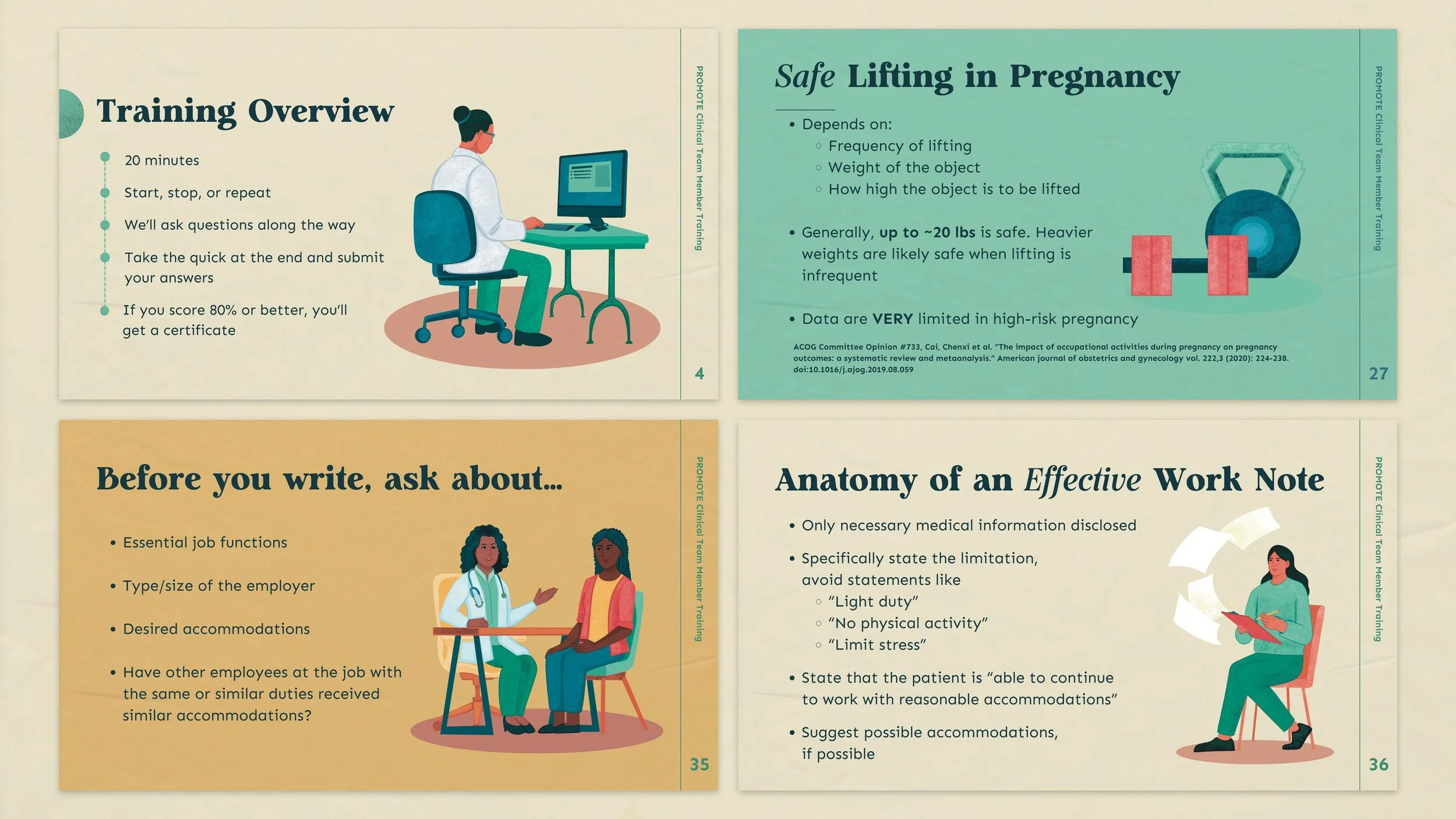
In this training that lasts about 20 minutes, we'll cover several important topics quickly. You can start, stop. Or repeat parts of the training as you need to. We'll ask some questions along the way to check for understanding, and at the end you can take a quiz and if you submit your answers and score 80% or higher, you'll get a certificate.
We'll start with the law, then move on to a review of the literature on workplace safety during pregnancy. We'll also cover dos and don'ts for providing documentation for an employer.
Let's start with the law. In section one, we'll review the federal laws that protect pregnant and postpartum workers in the United States.
While we are going to focus on the federal laws, there may be additional protections offered by state or local laws, or even by the patient's employer, so it's important to direct patients to additional resources as they're necessary. While there are several laws and statutes that may be applied based on the specifics of a case, we're going to cover the highlights of the most relevant federal legislation, the Pregnancy Discrimination Act of 1964, the Family Medical Leave Act of 1993, and the most recent legislative acts, the Pregnant Fairness Act, and Federal Labor Standards Act, or the Pump Act both enacted in 2023.
The Pregnancy Discrimination Act of 1964 prohibits discrimination based on pregnancy, childbirth, or its related medical conditions. That means there's a whole host of things that employers can't do legally to someone who is pregnant or may experience childbirth, for example, it's illegal for an employer to deny hiring promotion or to restrict work because of pregnancy or recent childbirth.
Importantly, the Pregnancy Discrimination Act also applies to people not only who are pregnant, but also to an individual who an employer thinks might get pregnant or who's had a past abortion. The Family Medical Leave Act or FMLA as most people know, it protects individuals from losing their jobs for 12 weeks when they take time off due to their own medical condition or to care for a family member.
FMLA provides up to 12 weeks of unpaid leave per year, and it can be taken all at once or as needed. Importantly, FMLA is only required to be offered by employers if the employer has 50 employees within 75 miles of the employee's website work site. And that individual employee has worked there, has worked at the company for at least 1,250 hours within the last 12 months prior to the start of leave.
As you can imagine, it can be challenging sometimes for employees to know whether or not they truly qualify for this benefit. The best thing to do is to refer a patient to check with their hr, their employee handbook, or a direct supervisor to determine their eligibility. This is also an important opportunity for them to learn about any additional protections or benefits that's offered through their individual employer.
There are several steps to requesting FMLA leave. The first step is that the patient should make the request of their employer for FMLA leave, and in general, patients are required to notify their employer at least 30 days in advance of an impending leave. They don't necessarily have to say the words FMLA or even disclose pregnancy at that moment.
However, they should provide enough information to let their employer be aware that they may have a need for leave. The second step is that the employer is obligated to notify that person whether or not they're actually eligible for FMLA leave and they're obligated to make this eligibility determination within five business days of the request.
Part of that process, the employer must provide FMLA rights and responsibilities, and they can also ask for a certification of medical condition from a licensed healthcare provider.
Next, we'll walk through a sample of what the certifying medical forms typically look like. Section one should be completed by the employer, and it includes the employee or in this situation, your patient's name, the employer's name, the date at which the medical certification is due. The employee's job title and their regular work schedule along with their essential job functions.
It's not uncommon that we receive forms when this section one has actually not been completed, and in that situation, it's best to ask the patient about their job title and regular job duties to guide completion of the rest of the form. Section two is to be completed by the healthcare provider or the healthcare provider team, and it's divided into three parts.
Part A typically asks for medical information. It will ask what time the condition will start, the best estimate of when the condition will end, and then the third question asks for more details about the specific condition. And then there's typically a box that allows the medical provider to identify that the condition is a pregnancy and to list the expected delivery date.
Part B of the healthcare provider section asks about details about the amount of leave that will be needed. In this section, the provider details, any planned medical treatments, referrals to other healthcare providers, and the estimated dates of time that the, that the individual will be unable to work or need accommodations.
Section C then asks about essential job functions and whether or not the employee is able, not able, or will not be able to perform one or more of their essential job functions. Most often requiring time off for medical visits or time away for a postpartum recovery is considered a period of time when someone cannot perform their essential job functions.
Once the employer has asked for a medical verification form, patients should return that form back to their employer within 15 calendar days after the employer's request. The employer must notify the patients of their FMLA status and if they're covered by FMLA, they must allow the person to come back to their position or an equivalent position after the F-M-L-E-F-M-L-A leave has ended.
The Pregnant Workers' Fairness Act is newer legislation that was enacted in June of 2023. Under this law, employers with greater than 15 employees are required to provide reasonable accommodations during and after pregnancy. A reasonable accommodation is a change to an individual's job that helps them keep working and does not cause undue hardship to the employer.
Reasonable accommodations will vary based on an individual's employer and their job description. Some examples are extra breaks, a sitting stool or allowing food or drinks at the workstation. You can imagine that something that's very reasonable in one job may be completely unreasonable for another unless there's an absolute medical contraindication to a specific activity.
It's important to ask your patient about their job duties. Prior to making suggestions about reasonable accommodations in general, your patients should have access to the same modifications that an employer has provided to any other employee in a similar position when they have a temporary condition that limits their activity, such as a broken leg or a sprained ankle.
Also, technically medical documentation from a provider is not ne, is not required. However, that may be very helpful to the patient. There is also federal legislation that applies to lactation. The Fair Labor Standards Act includes specific protections that are for lactation known as the Pump Act. Most employees have the right to reasonable paid break time in general.
That's about 20 minutes. And a private space to pump that is not a bathroom for up to one year. It's important to note that some specific employers are exempt. For example, railroads, airlines, and some small businesses with less than four 50 employees are exempt if a compliance would create an undue hardship.
Again, medical documentation typically isn't required. However, it can be helpful for your patients when a well-written work note is provided more to come on this. We've covered the most important federal employment laws that have implications for pregnant and postpartum workers. In summary, the Pregnancy Discrimination Act made it illegal to discriminate based on pregnancy or postpartum status.
FMLA protects a pregnant or postpartum worker's job for 12 weeks per year, but it does not protect their paycheck. The Pregnant Workers' Fairness Act mandates reasonable accommodations and the Pump Act mandates paid break time, and private space for pumping. Now, let's do a quick check for understanding the first question.
How long does FMLA provide unpaid leave for covered employees? Is it a five weeks B, 10 weeks, C 12 weeks, or D 24 weeks? If you chose C 12 weeks, you are correct, true or false? Break time for expressing milk should be paid for employees who are covered under the Pump Act. That statement is true. Break time for expressing milk should be paid for employees who are covered under the pump Act.
The challenge
U.S. employment law information as it relates to pregnancy, accommodations, and workplace protections is an area that is often misunderstood, outdated, dense, or difficult to apply in practice.
Duke OBGYN needed a training video that:
Clarified key employment law information for clinicians to minimize misinformation/confusion
Could be integrated into provider training workflows
Our Approach
We prioritized clarity and accessibility to ensure our audience could trust the content. We focused on plain language, thoughtful pacing, and avoided looking overly clinical, and disengaging. We understood that clinicians don’t always have long chunks of time to sit down for a training session, so it was important to break things up in an easy-to-digest format.
We designed a training video that helps clinical teams address:
Workplace protections during pregnancy
Accommodations and other employer requirements
Common misconceptions of patients and providers
Ways to support patients in workplace challenges
Escalating concerns and connecting patients with additional resources
Services Goodfight provided
Strategy and content framing for a clinician training video
Creative direction and scripting
Custom illustration system
Video production and post-production
Modular content designed for reuse across training environments
Video transcript
Welcome to Section two, workplace Safety during Pregnancy and Postpartum. I was just laid off yesterday due to my limits and restrictions from the doctor here. I was put on a 10 pound lifting limit, which is very, very small, and unfortunately with all the job descriptions at my employer, I wasn't eligible for employment anymore.
Data are limited in this area. We'll briefly review the literature about lifting, standing, and infection exposures. Data are limited in normal pregnancy and extremely limited in pregnancies affected by high risk conditions. We'll discuss the evidence-based principles, however clinical discretion may be appropriate in individual cases.
There are a few important things to consider when determining if lifting is safe for your pregnant patient. The first consideration is whether the lifting is frequent or infrequent. Keep in mind, frequent is generally considered more than once every five minutes. Therefore, most often when your patient is asking about lifting, they're talking about infrequent lifting.
The second consideration is how heavy the item is and how high the person has to lift the item. One important observation. Research has shown that for infrequent lifting up to 17 pounds is generally safe no matter how far along the pregnant person is, and no matter how high they're lifting the item.
Again. Importantly, these data aren't specific to high risk pregnant patients, and it's reasonable to use clinical judgment when advising patients with high risk conditions. For more information, we recommend that you review the ACOG Consult series number 7 33. There are limited data that are mostly poor quality observational studies that examine the association between standing and pregnancy outcomes.
Findings are mixed, and a recent review in meta-analysis published in Aja reports a link between prolonged standing, meaning four hours or more per day in preterm deliveries. The authors were careful to point out, however, that the quality of the evidence was low and the effect was very mild. Also, it is important to note that there is no link between prolonged walking and preterm birth in settings where a reasonable accommodation can limit standing to less than four hours per day.
That's ideal. If that's an essential job function, it's important to consider that these data are poor quality and the effect on birth outcomes was modest. It's also important to remember that overall exercises encouraged during pregnancy. And strict bedrest is associated with adverse maternal outcomes, including deconditioning, blood clots, and an increased risk of preterm delivery.
Employment in the medical and childcare fields are common among pregnant people. While no illnesses ideal during pregnancy, there are some infections that can be more dangerous. If we're all familiar with the classic torch infections when a reasonable accommodation can be made, ideally pregnant workers can avoid directly caring for individuals with active toxoplasmosis cytomegalovirus or CMV.
Rubella or varicella, which is also known as chickenpox. Personal protective equipment such as mask, gloves, and gowns are important as the source of infection may not be clear. Additionally, frequent handwashing is an important and effective strategy to avoid infections. Vaccination against flu, pertussis, and COVID can also reduce the risk of maternal or fetal illness and lead to improved health and fewer days of missed work.
Let's do another check for understanding safe lifting in pregnancy depends on all of the following, except is it A, the frequency of lifting? B, the weight of the object. C, the physical fitness of the pregnant person, or D, how high the object is to be lifted. The evidence-based answer here is C. While medical literature supports that the frequency of lifting the weight of the object and how high the object is to be lifted, nothing in the literature supports that.
The baseline physical fitness of the pregnant person is a major factor in determining what's safe lifting during pregnancy. True or false vaccination for influenza, tetanus, diptheria, and pertussis and COVID are safe and recommended during pregnancy. That's true vaccination for influenza, tetanus Dip theory, and pertussis and COVID are all safe and recommended during pregnancy.
Video transcript
In this third and final section, we'll talk about how you can write effective documentation when a patient is requesting a reasonable accommodations, or in rare cases when working is truly unsafe. They're supportive of me and they've been working with my accommodations. Right now I'm on a 25 pound weight restriction, so anything that would feel too heavy for me to lift or to move, they actually do it for me.
Before you write your documentation, it's important to ask about several key things. First, it's important to know your patient's essential job functions. Second, it's helpful to know the type and the size of the employer as that will guide whether or not the patient has access to several of the accommodations that we've talked about earlier in the training.
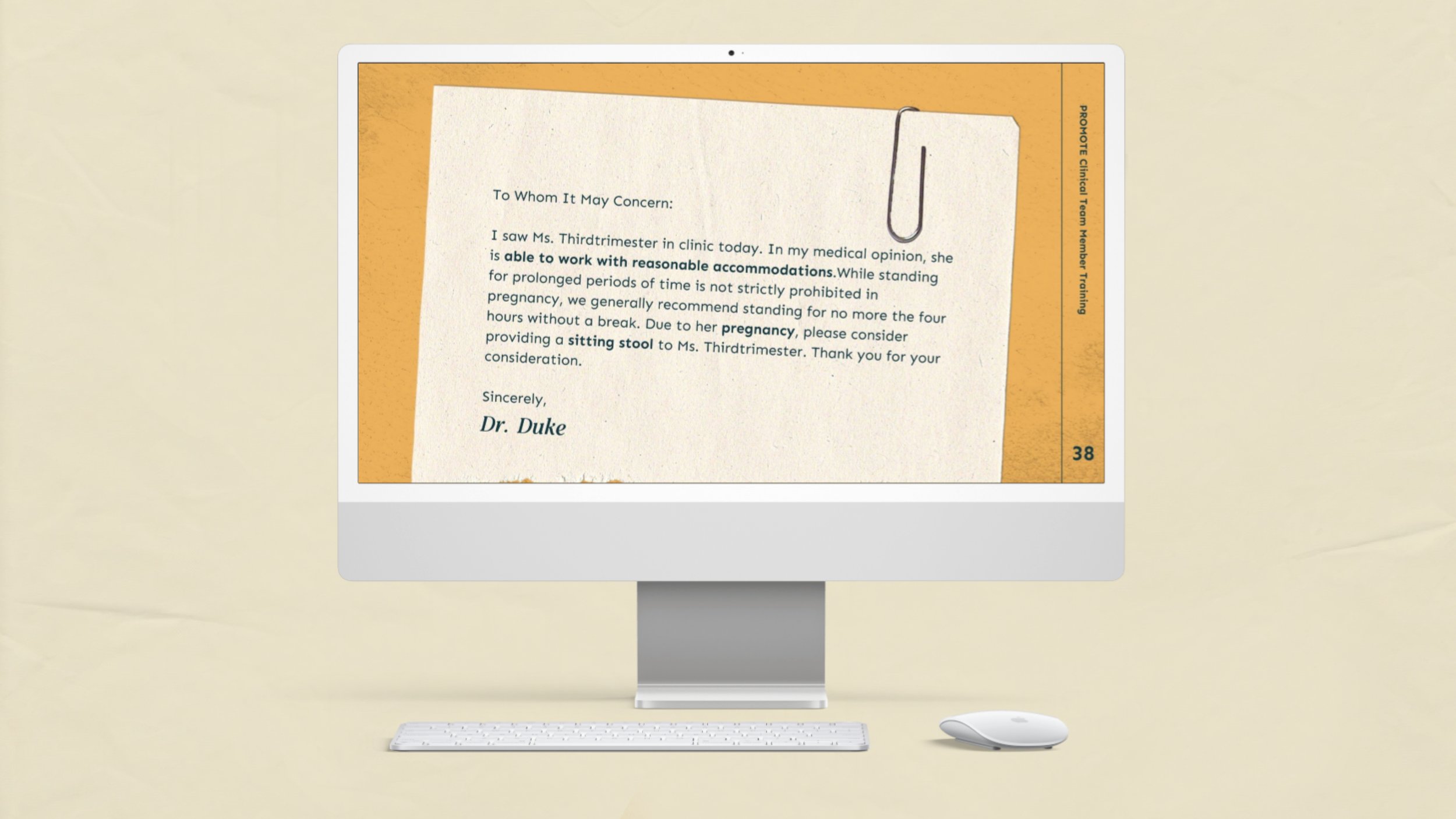
It's also helpful to know what accommodations the patient actually desires. One thing that can help to guide appropriate accommodations is to ask if other employees at their job in a similar or the same job duties have received accommodations previously. Let's talk about the anatomy of an effective work note.
The first consideration is that really only necessary medical information should be disclosed. Patients still have the right to privacy and recall that anything that a patient has not given approval to be disclosed should not be disclosed to an employer. It's also important to be very specific. You wanna state limitations directly and avoid any general statements like light duty or no physical activity or limit stress.
State that the patient is able to continue to work with reasonable accommodations and suggest possible accommodations when you have some reasonable ideas, particularly if those things have been utilized by that employer for other employees in the past. Let's look at some examples. Here's one example, to whom it may concern.
I saw Ms. Third trimester in clinic today. Please put her on light duty. Please do not hesitate to contact our office if you have any additional questions. Sincerely, Dr. Duke, the problem with this letter is that it's vague. It's very difficult for an employer to determine exactly what light, light duty means, and it would often be helpful to give some suggested accommodation.
Here's another example. To whom it may concern, I saw Ms. Th third trimester in clinic today. In my medical opinion, she's able to work with reasonable accommodations while standing for prolonged periods of time is not strictly prohibited in pregnancy. We generally recommend standing for no more than four hours without a break due to her pregnancy.
Please consider providing a sitting stool to miss third trimester. Thank you for your consideration. Sincerely, Dr. Duke. Here, this letter's quite different. One, the provider has clearly stated that the patient is still able to work with reasonable accommodations, and we've used that verbiage specifically because it comes from the Pregnant Workers' Furnace Act, and we've made specific comments about how long that person should or should not stand as long as it's not part of their essential job functions.
We've also tied this request directly to the pregnancy, which is important as that falls into the Pregnant Workers' Fairness Act, and given a suggested accommodation for Ms. Third trimester. While the laws that we've reviewed are important step to protect pregnant and postpartum workers, and forcing these laws can be challenging.
If a patient discloses to you that they've experienced discrimination or been denied a federally protected right, there are several places that you can direct your patient to for additional help. First, depending on the size and the structure of the company, human resources may be a helpful first step to correct the situation.
Some laws are new and direct. Supervisors may not be aware of their legal obligation, and HR may be a very helpful first stop. Speaking with legal aid is another option and may be a helpful first step if HR is unavailable or if there's concern for potential retaliation. There are free legal aid services available in many areas.
Finally, an individual can file a complaint with the Equal Employment Opportunity Commission or E-E-O-C-E-E-O-C. Investigations are often lengthy and by the time recourse is taken, the patient may have suffered lost wages and advancement ideally through appropriate counseling pregnant patients who desire can continue safely and comfortably working during pregnancy and when they return postpartum.
Let's do another quick check of understanding documentation to an employer requesting accommodations should include all of the following, except a detailed medical information about the patient's pregnancy. B, specific limitations or C suggested possible accommodations. The best answer here is a. While some medical information may be important, detailed medical information about the patient's pregnancy is most often unnecessary.
True or false, prolonged walking is associated with preterm birth. That answer is false. While there's some mixed evidence that links prolonged standing and preterm birth, prolonged walking has not been associated with preterm birth. Congratulations, you've completed the training. Let's see what you've learned.
Complete the final quiz, and if you score 80% or above, you'll receive a certificate of this training.
Built for Real Clinical Workflows
We sought out to create a training that provided flexibility to work through it self-paced, and in a format that supports onboarding, ongoing education, or quick refreshers. It can easily be fit into existing training routines across teams.
It works for providers:
Watching as part of onboarding
Using it during a department training
Coming back to it later on their own
Sharing it across teams to keep everyone on the same page
Our goal was to help providers feel confident while navigating patient questions.



Why We Fought for This Work
At Goodfight, we start with the why. This fight was about designing work that carries both clarity and care, so clinicians can step into employment law conversations with confidence and show up fully for their patients.
Working alongside Duke OBGYN, we led with alignment around what was at stake. When providers have clear, reliable resources, they can focus on the human moments that matter most. Conversations become more manageable. Guidance becomes more consistent. Care feels more supportive and more human-centered.
This project reflects how we approach every fight: getting the details right, communicating with clarity, and building visual systems that hold up in the real world. It’s the kind of work we do with clinical teams who are navigating complex challenges, and need tools that truly support the people they serve.

